How bad are the dermatomes?
Thanks for reading the 21st edition of my sciatica newsletter. This newsletter tracks my research as I write a book about lumbar radicular pain!
Today let’s talk about dermatomes. Dermatomes are a bit like special tests. They’re on every curriculum and in every textbook but they’re quickly falling out of fashion. Do they deserve the criticism?
Dermatomes were first mapped out at the end of the nineteenth century by the great neuroscientist Sherrington. To make his maps, Sherrington pinched the skin of rhesus monkeys which had undergone nerve root sectioning and established which areas of numbness corresponded to what sectioned nerve root.
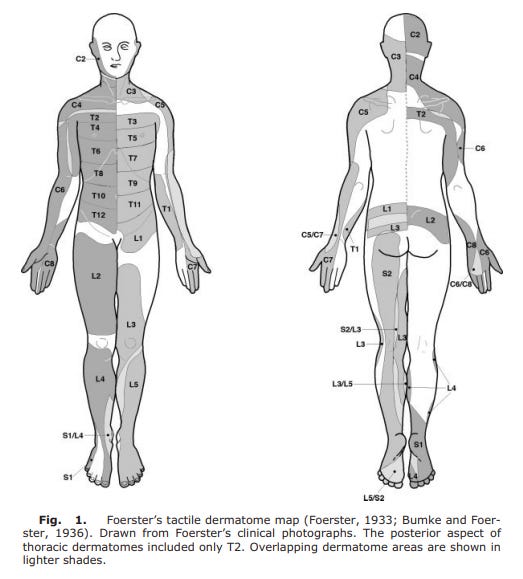
In the 1930s, the German neurologist Foerster drew out one of the two maps we most commonly use today by testing the skin sensation of his patients who had undergone dorsal nerve root sectioning as treatment for spasticity or pain. Foerster's map shows a patchy and irregular archipelago of dermatomes.
A decade later in the 1940s, Keegan and Garrett drew out the second of the two maps we most commonly use today, by testing the skin-scratch sensation of humans with disc-induced nerve root injuries. Keegan and Garrett's map shows an orderly and linear series of strips of dermatomes. It seems to be the most popular one nowadays.
The key point is that dermatome maps have always been of cutaneous sensation (hence the name dermatomes!), and not clinical pain. If we are using the dermatomes to diagnose radicular pain, we are using the wrong map for the territory.
(I do feel a bit sorry for Sherrington, for Foerster and for Keegan and Garrett, whose maps are now the subject of many a myth-busting "gotcha" blog post. As far as I can tell, they never made any claims that their maps were supposed to tell you where nerve root pain should be felt. And all these researchers emphasised, to greater and lesser extents, that their dermatome maps were simplistic and there was substantial overlap between their boundaries.)
How bad are dermatomes at nerve root pain patterns? Pretty bad. Let's look at some of the research. Taylor et al. asked patients with radiologically-confirmed L5 or S1 radicular pain to draw on a body diagram where they felt their pain. The composite maps of L5 and S1 pain were completely indistinguishable:
Albert et al. took a similar approach, and found that the composite maps drawn by patients did sort of correspond to dermatomal maps - but that for any one patient, a clinician could not guess the level of their lesion any better than a coin flip. Despite tough competition from Taylor et al., Albert et al. also win the prize for “creepiest diagram of a humanoid”:
Furman and Johnson asked patients undergoing an injection for radicular pain to draw out where the injection evoked pain. Even the pain patterns produced by this very specific stimulus were widespread, and varied between different people. Contrary to dermatomal maps, lesions at L3 and L4 caused pain at the back of the thigh as well as the front and lesions at L5 caused pain on the front of the thigh:
Only lesions at S1 seemed to cause pain resembling something like a dermatome map:
Finally, Murphy et al. compared individual patients' pain drawings to standard dermatome maps. The authors reported that pain was non dermatomal in two thirds of cases (Again, S1 was a notable exception: pain was non dermatomal in only one third of cases).
Why are dermatome maps so bad at showing where people with radiculopathy feel pain? The fact that they were never designed to do so explains only part of the reason. After all, one might still expect a nerve root lesion to cause pain in some sort of reliable, consistent pattern. I think there are a number of other reasons too, which conspire together to make radicular pain resist our efforts to map it.
Part of it is simply structural. A disc herniation does not always politely confine its contents to one spinal level. And nerves themselves are extensively interconnected. Some people have random connections between their nerve roots. Even inside the thecal sac, fibers from one nerve root can swerve out of their lane and join a neighbouring root. Of course, the ventral rami are jumbled together in the tombola of the lumbosacral plexus. And different sensory modalities - light touch, sharp touch, temperature - are relayed by different nerves and that those different nerves sometimes end up entering the spine at different levels.
And part of it is neurobiological. In response to a nerve injury, the immune system incites inflammation in the nervous system: neuroinflammation. Neuroinflammation lowers the firing threshold of local nociceptors so that they are more likely to cause pain. But neuroinflammation is not necessarily confined to the site of injury. As we have seen in a previous newsletter, people with radicular pain sometimes have neuroinflammation in their spinal cord. In this case, the firing threshold of nociceptors would be lowered not only at the affected spinal level but also at any levels that enter the inflamed part of the spinal cord. So an L5 nerve root lesion can cause pain at L4 and S1 if it triggers extensive enough neuroinflammation in the spinal cord. Animal studies and a few studies with humans have found that nerve root injury even causes the animals to become hypersensitive in the contralateral limb. Possibly this too is caused by spinal and supraspinal inflammation.
Okay, so the dermatomes are not good at mapping out clinical pain, and it’s not really their job to do so anyway. But are they good at what they are supposed to do: map out which nerve root supplies which area of cutaneous sensation?
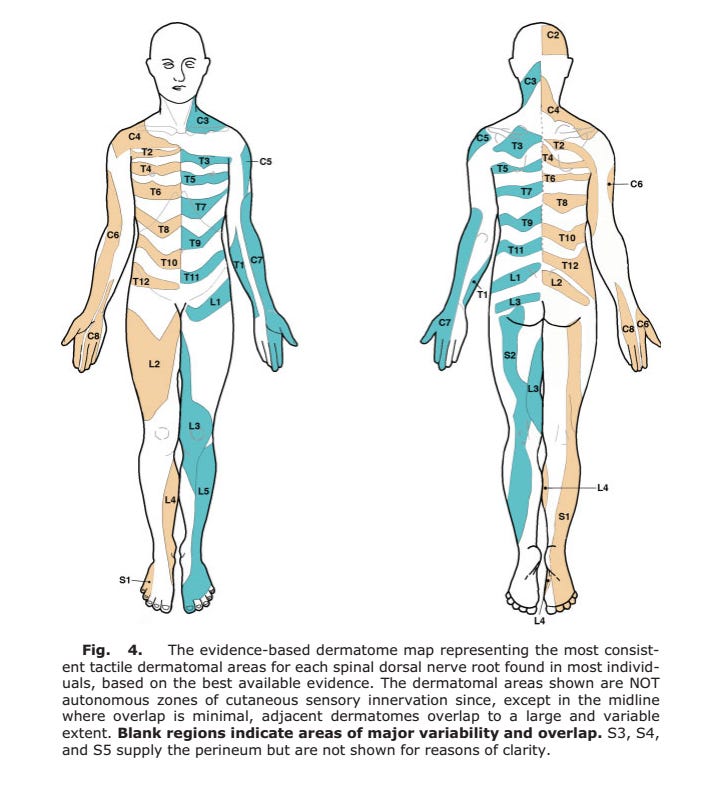
Sort of. To find out which parts of the dermatomes we can trust, Lee and colleagues carefully evaluated the evidence and came up with an "evidenced based dermatome map". In many ways, it does not look at all like the Keegan and Garrett map I am most used to. There is no evidence that the lower lumbosacral dermatomes enter the low back. L4 does innervate the medial calf, but it doesn’t swoop across the thigh and over the knee to get there. L5 isn’t long and striplike either.
But the S1 dermatome covers a long strip of territory similar to that reported by Keegan and Garrett (S1 proving reliable again). With some overlap, the L4 dermatome covers the medial shin, the L5 dermatome covers the dorsal aspect of the foot and the big toe, and the S1 dermatome covers the lateral and plantar aspects: not too far off what I am used to. I’ll be thinking of those next time I do a sensory exam.
We will find out if this “evidence based dermatome map” stands the test of time. What should we do in the meantime? I don’t think the dermatomes quite deserve a dishonourable discharge from clinical practice. Perhaps they just need a demotion to somewhere quiet where they can make themselves useful when needed, but mostly stay out of trouble.
That’s it for this week! I am still writing writing writing trying to get the first draft of my manuscript finished before Christmas. Tonight I’m going to play around with Adobe InDesign to see if I can format the book myself. I’m not sure how difficult it is. Let’s find out…
Til next time,
Tom
P.S. here are some photos I took of “the Mexican Eagle”, a caracara, which I saw at Anahuac National Wildlife Refuge last week 😊🦅













Well written, the textbooks better update their outdated dermatomal maps!
Curious if you also do neck pain?